Missouri’s new Nixon Forensic Center replaced a facility that predated the Civil War. In creating this modern mental health center, the design team had to balance maximum security and patient care while also facing challenging site conditions and program requirements.
After nearly 170 years in operation, Missouri’s Fulton State Hospital—the nation’s oldest state mental health institution west of the Mississippi River—has received a much-needed overhaul of its maximum-security facility. Over the years, various buildings on the forensic psychiatric hospital’s 52-acre campus had been constructed, renovated, and repaired to keep the site operational and safe. The term “forensic” refers to crime; thus, the majority of patients at the forensic hospital were “referred by the criminal courts, initially as incompetent to proceed to trial or as not guilty by reason of mental disease or defect,” according to the Missouri Department of Mental Health’s website. Eventually, though, these as-needed improvements were no longer adequate to meet modern standards at a facility that had been in operation since 1851 and was still using some buildings that predated the Civil War.
Most concerning was the hospital’s high rate of workplace injuries, which led to lost time for employees, cost the state $4 million annually in workers’ compensation, and created difficulties in recruiting and retaining staff. A December 2013 report for the state, titled Rebuilding Fulton State Hospital, noted that it was “far more dangerous” to work at the psychiatric hospital than at a corrections facility.
As a result, the Missouri Department of Mental Health decided to rebuild the entire facility, leading to the creation of the $211-million, 300-bed Nixon Forensic Center in Fulton, a city 20 mi northeast of the state capital, Jefferson City. The new facility was renamed in honor of former Missouri governor Jeremiah “Jay” Nixon.

Today, the Nixon Forensic Center is a state-of-the-art psychiatric hospital that provides a safe and secure environment for patients with serious mental illness who have been committed by Missouri courts for evaluation and treatment. It specifically replaced the services provided by the state hospital’s Biggs Forensic Center, an adjacent, maximum-security facility constructed in 1940. Deemed unsafe for patients and their caregivers, the Biggs center was a multifloor facility, requiring patients and staff to use stairways. This, combined with the building’s short floor-to-floor height and its tight, difficult-to-secure spaces, presented problems for patients and staff. Also, its concrete-block bearing wall construction was not conducive to reconfiguration, so remodeling was never a practical consideration. In multiple ways, Biggs had outlived its purpose.
The international engineering firm WSP USA became involved in the Nixon Forensic Center project in 2014 when the design was awarded to the team of WSP—as the prime consultant, especially for key portions of the structural engineering—and EYP Inc., as the design architect. Working in collaboration, WSP and EYP led a team of architects, engineers, and psychiatric care specialists to design the new hospital. The project team worked with the state’s project managers, which included Missouri’s Office of Administration Division of Facilities Management, Design, and Construction (OAFMDC). David Mason + Associates was the civil engineer and worked on the structural engineering. River City Construction was the general contractor.
The design process began with an examination of the Biggs Forensic Center to gain a general idea for the programs and spaces required in a new facility. The design had to strike a balance between being a caring, healing, therapeutic environment and secure infrastructure that would reduce the risks of patients harming themselves or their caregivers. For example, in contrast to the Biggs center’s multiple floors, the main hospital portions of the new facility were designed as single-story buildings, covering roughly a quarter-mile length. Other sections of the new complex are two or three stories tall and include attic space used to distribute and maintain mechanical and electrical services from outside the secure patient area.

A town-hall-style meeting with hospital staff and patients helped the design team gather valuable information from the people most impacted by any design decisions. A series of workshops provided further opportunities for the design team to interact with caregivers, administrators, clinicians, and plant operations personnel.
Continuous collaboration over an 18-month period was critical in setting the course for programming, planning, and designing the facility. This effort was an iterative process between user and designer to discuss goals, objectives, and needs and then in turn, review concepts, plans, and renderings as the design unfolded. The hospital’s staff was consulted to help reach a consensus before proceeding with design concepts.
A WSP web-based file-sharing program provided a common repository for all documentation that enhanced project communication. Likewise, a web-based Revit central file system, manufactured by Autodesk Inc., allowed all consultants to review and work on the hospital’s building information model to develop the design and construction documents. That spirit of open communication continued throughout construction, with monthly project site meetings attended by the OAFMDC construction representative, WSP’s construction representative, the contractors, and the consultants.
The existing Fulton campus housed essential functions that had to be retained until the replacement facility opened. So design and construction were phased to allow ongoing, uninterrupted operations. For example, the central plant that provided steam for heating, chilled water for cooling, and hot water was on the eastern half of the site. The central kitchen, materials management, laundry, and maintenance shops were located there as well as the administration building, vocational center, and several storage buildings. Thus, five enabling projects to maintain ongoing operations were needed before construction began.
The first projects included the design and construction of three boiler plants to provide heating and hot water to the buildings that would remain, which were previously served by the central plant. Next, a services building was constructed that included a central plant, kitchen, materials management, and maintenance shops. Once that was completed, the general contractor commenced with the abatement and demolition of the buildings, roads, and tunnels. When that was settled, construction of the new hospital began. The plan was a success with no disruption to hospital operations during construction, and the safety of the workers, patients, and staff was a top consideration throughout.
In plan, the new complex features a series of long, rectangular structures that serve as the administration building, the treatment center building, a medical and vocational center building, and a new central plant building. Together with two long, slender curving corridors, these structures enclose a series of courtyards that provide space for recreation, meditation, and other activities. The corridors also provide access to the living units for the patients—six structures with a form based on Japanese fans, each housing two units (see “Secure Structures”). Although the various interconnected elements appear to form a single, enormous building, each structure is actually separated from its neighbors by expansion joints.
Key areas within the Nixon Forensic Center include seven unique spaces:
• the Brandt Vocational Center, a place where patients assemble products such as ventilator masks or sell baked goods and which is divided into three areas that can be used individually or collectively
• the Hope Center, a treatment “mall” where patients go to attend classes, shop, bank, recreate, attend religious services, or work out in the main gym
• a medical clinic, where patients get physicals, see dentists, are examined by medical specialists, attend physical and speech therapy, see optometrists, or if ill, are treated in a small inpatient hospital with four rooms
• four treatment program community rooms, where patients attend small and large group therapy sessions and classes and visit with psychiatric specialists
Each of the 12 living units provides space for 25 patients. The units are clustered around the Hope Center and are monitored by a pair of nursing support areas designed to save space, improve functionality, and provide for security backup from the adjacent unit in crisis situations. Each living unit is assigned to one of four specialized program communities, where patients with similar psychiatric issues receive specialized treatment. The program community approach is a unique clinical element for the facility and considered the first of its type in the country.
The forensic center layout was designed to eliminate blind spots. A central nurses’ station in each living unit provides staff with a clear sight line to each patient room, treatment site, office, and restroom door. The nurses’ station was custom-designed to address both security concerns and a desire for openness to the patients. This design included a raised and widened counter and an increased horizontal depth of the station, so that patients would be unable to reach into the nurses’ station, potentially gaining access to staff or the patient room-monitoring systems.

Overall, the hospital’s architecture creates a therapeutic environment. The corridors that connect the living units to the therapeutic communities are gently curved to avoid tight spaces and blind alleys and to reduce the apparent length of travel. The interior finishes and fixtures were selected for their durability, timelessness, and safety. It was important that the design did not include any finished items that could be crafted into something dangerous to patients or staff. The design of the corridors and all patient spaces emphasizes the use of natural light and views of the exterior, in recognition of their therapeutic importance.
In addition, all mechanical, electrical, fire protection, and telecommunications systems are distributed overhead through a secure system that allows mechanics to work on the heating, ventilation, and air-conditioning, fire protection, and electrical systems without interacting with hospital operations below.
It was challenging to design a building that evaluates every detail as a potential ligature point—something used for tying or binding a cord, rope, or other length of material—especially when creating a normative therapeutic environment. There could not be any places where even something as fine as dental floss could be anchored and used to injure oneself. Moreover, designing a hospital that provides disaster protection to patients who do not have the freedom to leave the campus requires a special understanding and practical application of building codes and life-safety codes.
Although the Biggs Forensic Center, located across a street from the new hospital, is slated for demolition, some existing buildings on the campus will be retained, including the Guhleman Forensic Center, for patients convicted of sexual predatory crimes; the Hearnes Center, currently used as an administration and training center; and the Department of Corrections’ Cremer Center, a stand-alone penitentiary for people with drug and alcohol dependencies.
Because the site conditions required a massive regrading effort to accommodate a 60 ft change in elevation (see “Civil Support”), finding suitable soils in the cut sections that could be used as engineered fill elsewhere in the project was a challenge. The geotechnical reports from TSi Geotechnical suggested that good material was available, but locating it proved to be difficult for the contractor. By using a combination of building demolition debris and available non-expansive soils, it was possible to place suitable building pads beneath the new construction. In areas where older buildings were demolished and tunnels removed, the soil was exposed and then weakened by rainfall and runoff. The contractor was permitted to use building demolition materials in the excavations to provide stability. But no demolished material larger than 4 in. in diameter was permitted, and none was allowed within 2 ft of a foundation or slab on grade. Retaining walls were used on the lower part of the site to provide a suitable building pad. The high side of the site was banked with a slope that stayed within Missouri state requirements, which limit banks to a maximum slope ratio of 3:1.
Most of the new buildings are founded on conventional spread footings at depths of 3 ft. But the columns for the facility’s three-story administration building on the western side of the hospital are founded on drilled piers. The Nixon Forensic Center does not have basements or underground levels.

A key project goal involved reducing energy costs. With that in mind, a hot water boiler and chilled water plant were installed to provide efficient heating and cooling for the facility. The ductwork and other infrastructure for these systems, along with the communications, fire protection, and security systems, are located in attic spaces above key parts of the facility, including the living spaces and the curving corridors that lead from the south end of the services building to the north end of the administration building. For security reasons, these attics cannot be accessed by anyone in the areas where patients are allowed; only maintenance staff can enter the spaces from outside the secure perimeter.
It was a challenge to install straight sections of pipe along those curving corridors while also maintaining the necessary clearance for maintenance staff to walk the path adjacent to the piping. A second challenge involved the distribution of air from the mechanical room in the attic above the living units to serve the individual fan coil units (FCUs) in the patient bedrooms below. This was especially complicated because of the need for staff to change the filters and maintain the FCUs without entering the living units. To accomplish these goals, the FCUs themselves were installed in the attic spaces and individually ducted to each patient bedroom.
A solar hot water heating plant was located on the roof of the services building. This plant preheats all hot water, which is stored in insulated tanks within the services building. The water is distributed to plumbing fixtures through a heat exchanger that heats the water to a safe temperature for showers and handwashing.
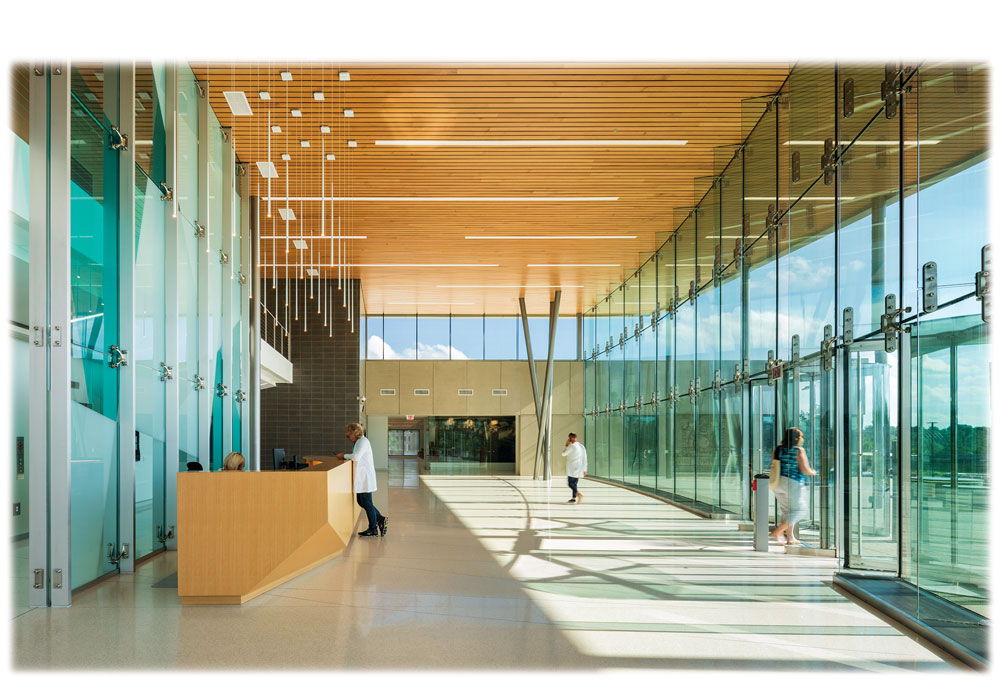
In addition to solar thermal arrays and solar storage tanks, the project’s sustainability aspects use natural light wherever possible. For example, natural lighting is used extensively in the corridors, living units, therapeutic areas, and administrative spaces. The corridors feature large expanses of impact-resistant glazing to provide daylight and views from the corridors into the surrounding network of outdoor courtyards. A common, open space called a day room in each living unit is lit by an overhead clerestory that admits diffused daylight. Each patient room, office, and therapy room within the living unit is also provided with daylight and views through secure windows.

The administration building features a glazed curtain wall on its western facade that provides daylight and views from the internal circulation system. The space features a three-story open stair that enables staff to move from floor to floor to promote wellness and reduce reliance on elevators. The glazing on this west elevation is high-performance glass with ceramic frit patterning to reduce solar heat gain, balanced with vertical sun shading and terra-cotta cladding.
The main entrance is through a two-story lobby protected by a generous canopy, which provides daylighting and views while minimizing solar heat gain and glare.
Construction of the one-story services building began in April 2015 and was completed in May 2016. Hospital construction started in 2016 and was substantially completed in May 2019. Patients moved into the new hospital in July 2019.
The facility’s state-of the-art, responsive design represents a direct reflection of the clinical staff’s treatment strategy and programs. Ultimately, its success will be measured by a reduction in staff absenteeism and short- and long-term disability claims, an increase in the ability to find qualified staff, a reduction in patient self-harm, and the successful treatment and ultimate discharge of patients. Many of the planning ideas implemented in the Nixon Forensic Center can be carried into the design of future forensic psychiatric hospitals.
PROJECT CREDITS Owner State of Missouri, Department of Mental Health, Division of Behavioral Health Prime consultant WSP USA, St. Louis, office Design architect EYP Inc., Washington, D.C. General contractor River City Construction, Ashland, Missouri Civil and structural engineering David Mason + Associates, St. Louis Mechanical, electrical, plumbing, fire protection and communications engineers Mazzetti/William Tao & Associates, St. Louis Geotechnical consultant TSi Geotechnical, Olivette, Missouri Health care architects Heery International Inc., Iowa City, Iowa Behavioral health care consultants Marc Shaw Architect LLC, Arlington, Virginia, and Joel A. Dvoskin, Tucson, Arizona Perimeter security consultant Latta Technical Services Inc., Plano, Texas Landscape architect Kathy Williams & Associates, St. Louis Environmental consultants United Infrastructure, St. Louis, and SCI Engineering Inc., Saint Charles, Missouri
This article first appeared in the September 2020 issue of Civil Engineering.